
How Am I? An Update on Dragging Along with Primary Biliary Cholangitis (Cirrhosis)
Roughly a year ago, I said, I’m done. No more pricks or scans. Longtime readers will know that my life from 2010 to 2015 had become a gruesome slough of gastric/esophageal varices bleeds, an uncommon complication of early and mid-stage cirrhosis (not so uncommon in end stage). My labs were never that abnormal during this period, so I was diagnosed with every weird ulcer subspecies in the field guide. Not until I had a shunt [TIPS] put in my liver in July 2015 could the portal hypertension be measured, and it was high.
I announced I was going to quit writing about this, but I get occasional questions, and I may as well keep the history going.
I have had no more bleeds, and that is a very good thing. I think the encephalopathy which followed had some lingering effects. My spatial sense isn’t what it used to be; I can go to the drugstore, which requires exactly one turn, and end up going in a circle. Subtraction of 3-digit numbers is hard. Short term memory isn’t too keen. I haven’t had any recurrences, and I think this is attributable in large part to eating absolutely no red meat or pork. But the fatigue, which is the most common complaint of people with PBC, seems worse.
It is hard to explain because it is not everyday tiredness. It doesn’t matter if I sleep 12 hours, after being up an hour or so I am going to be tired. I can press through, and a really active day is one where I go out to breakfast, walk the dog, and go to the store. I’ll pay for it the next day when I will be too tired even to read. Maybe if I did more, I would feel like doing more, you might think. But 2 days on is going to mean 2 days off, and 3 days on will be 3 off, and at some point I will quit enjoying being on, so if I don’t have to, why not stop?
Remember The Roadrunner cartoons when the coyote is squashed by a boulder, peels himself off the pavement, and then an Acme truck comes barreling down and pancakes him again? It is like that. Still the coyote keeps chasing that roadrunner.
I vacillate between gratitude for every day — for security and safety and a loving husband who picks up my massive slack —, and weariness. Facebook can get to seem like those wretched newsletters people would send out with their Christmas cards, where all reports are of visits to exotic places by people who are legends in their own minds. Good on them. But Christmas newsletters came just once a year.
Since I don’t go out much, the feeling of being an alien increases. I look at these reports from a distant place. Stay out of a big box store for a year. Then visit. Lord, how much stuff there is. Who could possibly need this much stuff? I’ve bought one pair of shoes and one dress in the past three years.
Goodness me, how much time and money people spend on food. So much of social life seems predicated on food and alcohol, which I simply treat as something in the category of never again. The most annoying problem I have may or may not relate to the PBC, but finally I have an appointment with an esophageal expert. It’s been going on for years. I’ve had the standard three tests for esophageal motility, but results were negative, no problem. I don’t care what the results of these swallowing tests conducted only with liquids are. It is not normal way too often to be able neither to swallow food all the way or get rid of it the opposite way. My hepatologist agreed (hurrah!). I eat a lot of refrieds with rice. Smooshy and a fair protein source.
So yes, I did go back to have another set of sticks and an ultrasound done. I decided it would be stupid not to check on the TIPS. The TIPS is functioning; “patent” is the word of choice. The real time ultrasound had been going on for 40 minutes when the sonographer left to fetch the radiologist himself. There were veins she just could not find. Apparently, I have a strange body architecture.
At the appointment the next day, the hepatologist asked that I return for a CT scan. We had planned a trip to the beach, and went ahead, and I sat on the dunes and thought, isn’t this just dandy.
Then Monday I had the CT scan, which looked as expected, except for “small” varices in the stomach. Dear god. “Varices.” I thought I would never have to see that ugly word again.
Most people with PBC don’t haven’t problems with bleeds. A tiny number who have the shunt installed do develop gastric varices. Most of this little pool do not have varix bleeds. I don’t want to be a footnote to a footnote to a footnote. Neither will I be terribly surprised if I am one.
Beware of “Bubble Soccer” or Knockerball

There’s a new craze in the sports world that PTAs, principals, parents, EMS, ER personnel, orthopedists and neurologists need to be aware of.
It goes by the deceptive name “Bubble soccer” [also Knockerball] and the claim is that, how can you possibly get hurt in a bubble (like wrapping your child in bubble wrap!). Plenty of ways, it seems, especially if those outfitting and presumably monitoring the players are ignorant about its dangers.
It doesn’t help that ER personnel greet their first cases with a smirk: so you managed to hurt yourself wrapped in a bubble?
From the videos I have watched,* I have seen very little soccer going on. Rather, the playing field looks like a lot of people playing bumper cars — without the cars, like a freeform smash-up. What could possibly go wrong?
Some suppliers are themselves concerned about unsafe practices:
“It may be ignorance or negligence, but either way, it’s incredibly dangerous. Consider [May 2016] this brain injury incident in Atlanta that was caused by a collision like this one. In both cases, the equipment was extremely unsafe and should never have been used. We have seen equally dangerous bubble soccer in San Diego.”
Six months later the Emory University neurologists who treated the player mentioned above published “How safe is Bubble Soccer?” in the Journal of Clinical Neuroscience.
Then there is this one (spring 2017) from North Alabama: “Shoals student suffers severe brain injury playing Knockerball”. I don’t know if he survived or is paralyzed like the man who won $45 million from a Missouri Knockerball franchise.
Risk Assessments can be revealing:
https://www.vertigozorbing.co.uk/wp-content/uploads/2018/03/risk-assessment-body.pdf. Note the overall-risks are highest when staff are negligent. Untrained or unvigilant party-rental staffers are not the type of people best equipped to protect your or your child’s safety.
Youtubes: Even when supervised, the potential is there: https://www.youtube.com/watch?v=PkJdTwgGnU8.
In addition to risks for arm and leg breaks, whiplash and torn ligaments, when the head is jostled around, concussions occur. The marketing site Mindful Marketing provides a stern warning (“Concussion Ball?”) on the dangers of this “self-regulating” (we know what that means) sport.
You can search any metropolitan region and see ads aimed at summer camps, the birthday party market, school field days, and church groups from party rental companies. They may have enough years behind them that they can manage ballpits for elementary kids, but would you trust them with the kinds of issues noted by the Risk Assessment above?
One school system won’t. Remember, this craze is less than two years old. It has already been prohibited by the Fairfax County Schools in Virginia. This district is a bedroom community for Washington DC and thus I imagine has a fairly high rate of lawyers per capita.
They know a potential liability suit when they see one.
It’s the traumatic injuries that make the news and the medical journals. But if there are traumatic ones, it’s a good guess there are lesser ones, and comments are invited.
*This one is from the Knockerball website; it is the game as it should be played with adults who aren’t trying to hurt one another. I think Fairfax County Schools considered, if this is the best, what would be the worst? What happens when the kids have aggression to release and vary widely in height and weight? What happens if one shows distress and a teacher suits up to investigate? Wham, that’s what.
Photo Attribution: By Julkina – Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=39183682
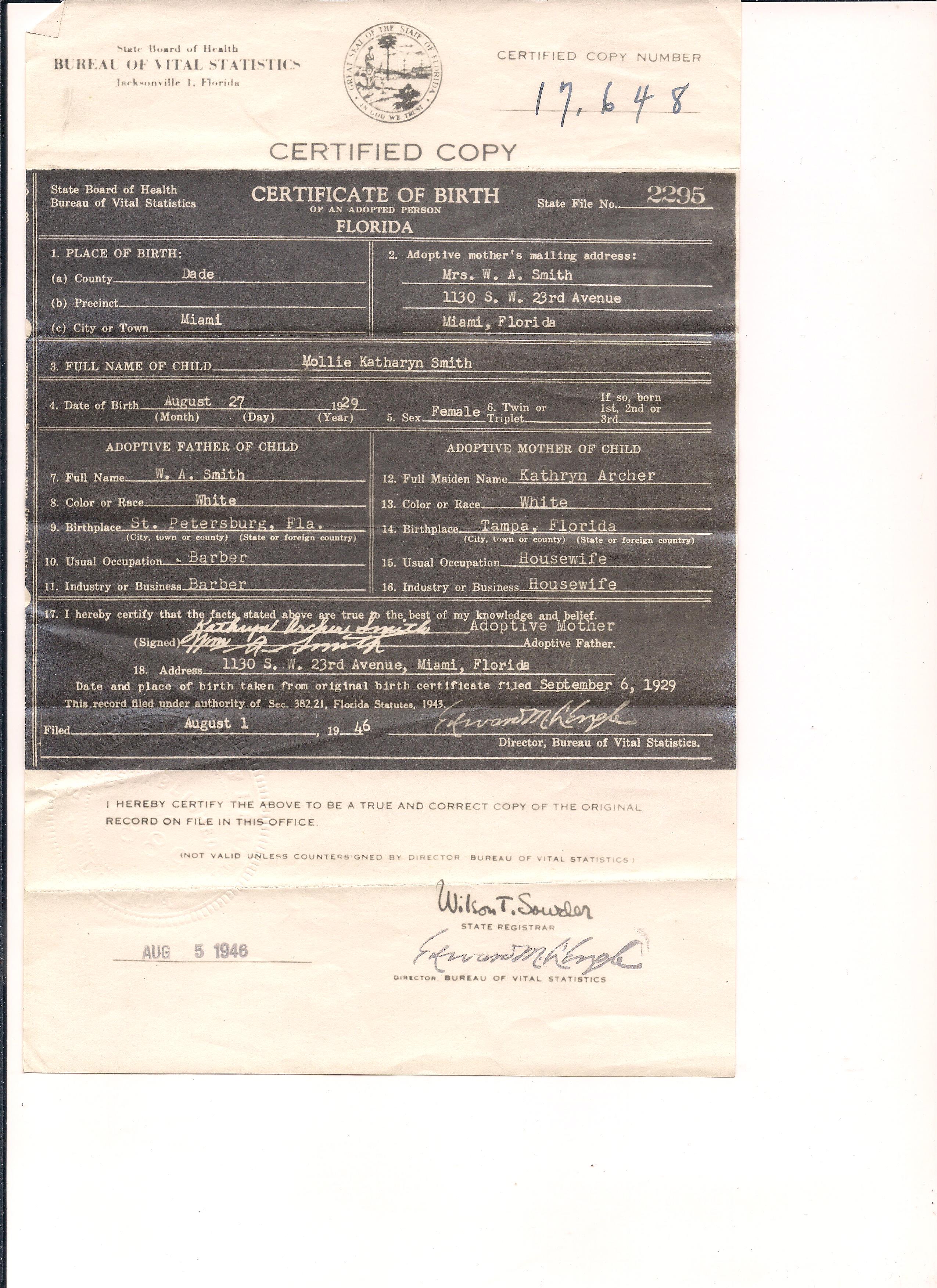
Birth Certificates of Patricia Ruth Millard, daughter of Lucile Millard (b. Ernstine Millard)
I’m putting these up because I may be the only person who has the physical objects. In 1929, when my mother, who was given the adopted name Molly Kathryn Smith, was born on August 27, 1929, the State of Florida permanently sealed adoption records.
Through sheer persistence my mother induced a clerical error in the 1960s and attained the birth certificate listing her bio-parents and spent the next decades tracking down her numerous aunts and uncles, none of whom was surprised by her existence, and, varying by physical and emotional distance from her birth mother, their sibling, accepting or not.
All this was done without the aid of the internet. I have found it difficult to go into existing genealogies on the Church of LDS or ancestry.com to update because the assumption seems to be that an adoptee gets a line — but had no past, and, since his/her bloodlines would not connect to bloodlines of the tree on which he or she appears, no future.
So for the sake of searchers, allow me to chronicle this here, since according to the State of Florida, the bio-birth certificate is for their eyes only. Patricia Ruth Millard who became Molly Kathryn Smith, had three children, two males and one female, all still living, and a son and a grand-daughter without issue. She died in Buncombe County, NC 7/8/2015.


My Miami
My mother was born in Miami in 1929 and my father arrived at 3 months in 1927. I was born at Mercy Hospital on Biscayne Bay, Coconaut Grove, Miami. I never lived permanently in Miami after I left home in 1976, but my parents did.
My mother grew up hearing her father’s stories of the 1935 hurricane when so many Miamians took boats into the Keys to recover the bodies of those who lashed themselves to trees, like mariners to masts, hoping not to blow away.
They didn’t. Instead, they drowned.
The 1960s and 70s were fairly quiet decades for hurricanes, after Donna in 1960. The only category 3 or higher I remember was 1965’s Betsy. We boarded up the windows — which means just what it says, covering with boards.
Then the part my father hated: stripping the two avocado, mango, and grapefruit trees so that the fruit would not become projectiles.
The power went out; it was very dark and we just sat and listened. I don’t remember the heat, but in 1965 we didn’t have air conditioning (and always only had wall units). Then the radio and sounds outside agreed we could emerge. A lot of trees had been blown down, and the neighborhood men worked together to clear them out of the road.
My childhood home, just west of Coral Gables and 6 blocks south of Calle Ocho (SW 8th street) was built in 1947 and my mother claimed that the rectangular concrete blocks had been turned at 90°, making the walls effectively twice as thick. The house was built in 1947; my parents bought it in 1961 (by that point the carport had been turned into a living room. Not a fancy house, but strong.

Notice that it had a solar water heater in 1947! My parents went through Andrew and Katrina. The roof was (eventually) replaced after Andrew.

By the time it was sold it in 2014, the yard was so thick with foliage you could hardly see the house (the subdivision had once been a dairy).
But they never evacuated or sheltered. Neither did any of my friends’ families. Neither did my grandparents. It was never seriously discussed. Why? The history of the structures.
They were built on solid ground, not drained swamp. They were appropriately designed for the tropics, with thick concrete walls and low pitched roofs. They were inland by a few miles at least. My parents had a healthy respect for hurricanes; they simply trusted their own home more than they did the government shelters.
My mother’s parents’ house looked much the same when I last drove by it in 2013 as it does in these pictures. I thought it fantastic because if had two stories. It is a frame house, with very deep porches, in the Shenandoah area (now Little Havana), less than four miles to the bay. I believe that the point of such deep porches could have been to take the brunt of lashing rains coming from the east.

Later the palm tree was cut down, perhaps to prevent an uprooting and crash on the house. 
I don’t have a good picture of the house my father grew up in; by the time I came along, it was my aunt’s. I know it was still standing well into the 2000s. It was likely made of limestone or concrete. Some of the houses in Coral Gables were built of coral.
What will Miami look like tomorrow after Irma? A mess. The question is what will the houses built before Andrew and after the 1960s boom look like? And those not built on solid ground, but on drained swamp? Or close to sea level?

Goodbye to all that: No more sticks. No more scans.
I never intended for this to become an illness blog, but once I became symptomatic for the Disease Formerly Known as Primary Biliary Cirrhosis, I could find no narratives of what to expect, and so I decided to chronicle my mess.
Last month I told my hepatologist we were done here. No more scans. No more sticks. There is no point in watching the numbers because there is only one way to possibly delay dying: a transplant.
Don’t fret; there is no reason to believe I won’t be around a while. But I have spent too long seeing my life as a slo-mo train wreck.
I felt tremendously free after announcing the end to tests. He said now my MELD was 15, it was time to start thinking about getting on a transplant list. I told him no, it was not.
I’d known this day was coming for 11 years. I had been ambivalent about it, but these are the reasons I told him no. (He said I can always change my mind). I don’t advise anyone else to take this route. If my children were younger, I would not.
- There’s a fair chance that after a year or so, the autoimmune illness PBC could come back with a vengeance.
- I don’t want to spend the rest of my life on immunosuppressants.
- Some programs require you to re-house your fur people. Our household includes 3 cats, 2 dogs, and 3 ferrets. Those cats and dogs aren’t going anywhere. (The ferrets stay on the top floor with my daughter.)
- Even if all went perfectly (not the way they usually do for me), a transplant would start at $150,000. They can easily end up costing $800,000+ range. Even if my insurance coverage doesn’t change in October, it would only pay for 80% of the cost. So we are looking at a minimum of $30,000. While we could swing this, we could not do the upper range without accruing enormous debt. My husband would be willing to do whatever it took, but I am not willing to see his life or our daughter’s (who is still in school) complicated by such a huge gamble.
- I’m not entirely sure that on a spiritual plane donors are dead.
I think my hepatologist might have been relieved because it saved him telling me I may not be a candidate since in between this and my previous visit I had been diagnosed with a severely enlarged left atrium. Hearing this was a bit of a relief since it means that I could drop dead and miss all the liver failure gore.
So how am I? I’m tired, all the time. This could have much to do with the heart and little with the liver, or both working against me, not to mention a whacked auto-immune system.
The worse thing is likely unrelated, although it remains unexplained in spite of every test in the box. Too often I have “steakhouse syndrome,” even with macaroni. So even eating is not pleasurable any longer.
But I can still read, so I am fine. I don’t get out much but I have an active cyber-life.
I’m sick of being sick. If anything interesting happens, I’ll post. Otherwise, I’d rather write about something–anything–else or not at all.
Who Knew a Photographer from Getty Images Went to the Moon?
“It is unlawful to falsely claim copyright or other rights in NASA material.” — from the NASA Media Usage Guidelines
So how does Getty Images get away with licensing pictures from the moon? Wouldn’t “other rights”include licensing? Maybe the judge reviewing the Carol M. Highsmith case can cast some light on this.
Go to the search bar on the Getty Images opening page, and enter “Apollo 11.” Here are a few results (“Apollo 11” yields 81 pages):

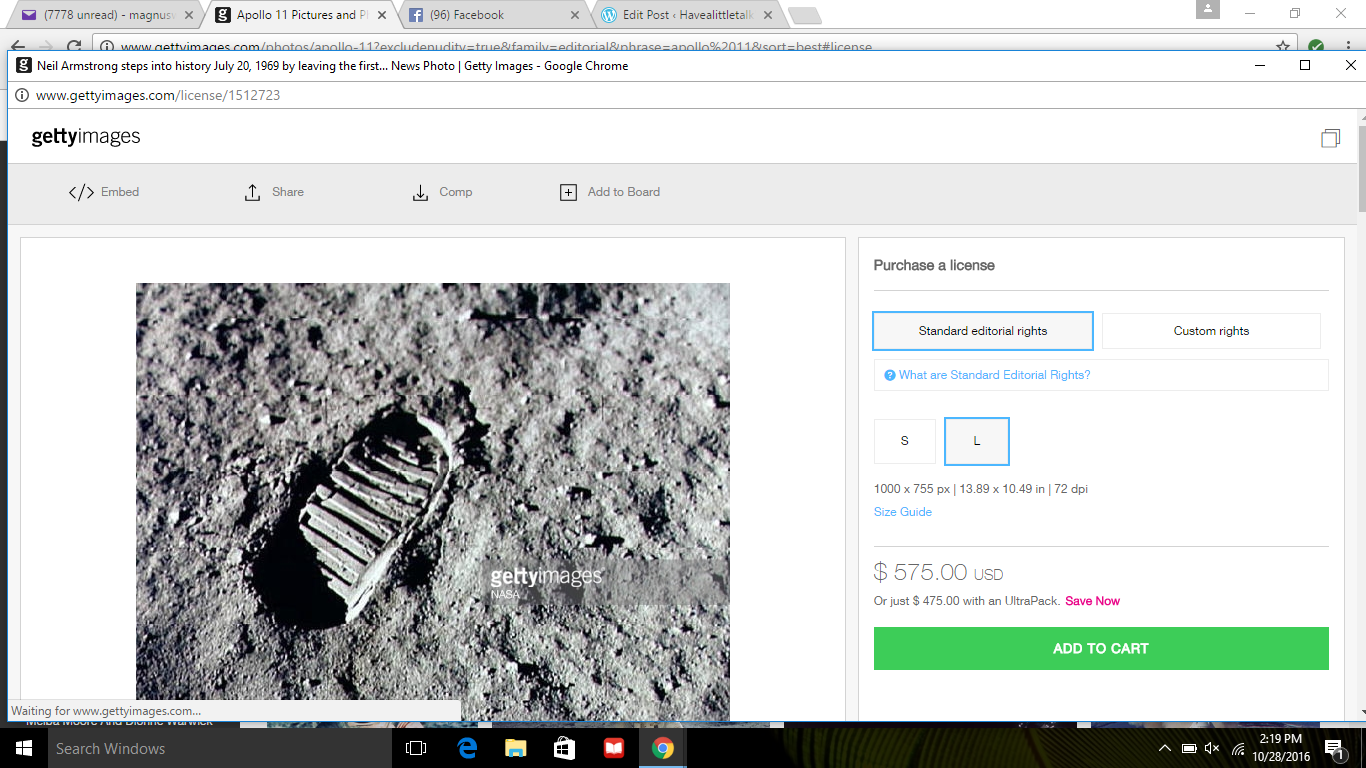

Now go to Google and search for “Apollo 11 Images.” Click through any of the image results that specify NASA.gov as the domain, and it won’t be long before you will find your way to the Apollo Archive of NASA, where there are 724 images for Apollo 11 alone.
All three of these pictures, and many more that Getty is trying to license for use at $575.00 a piece, are available to download free at the Apollo Archive.
The astronaut is Aldrin. Control number at NASA is AS11-40-5903.
The bootprint’s NASA ID is AS11-40-5877 or AS11-40-5878.
The moon (“view of full lunar disc during return trip”) NASA ID is AS11-44-6667.
Cost to download these images from NASA: = $0.00.
Gettying: How Getty Images Charges Users for What They Already Own
A few weeks ago, I posted “The Audacity of Getty Images: Exploiting Carol Highsmith, America’s Photographer” about the way Getty Images took from the Library of Congress thousands of images placed in the public domain by “America’s photographer” Carol Highsmith. Her intention was that Americans could use them without paying a cent. Getty downloaded these images from the Library and then uploaded them on its own site, Getty Images, and charged licensing fees for using these pictures, which belong to them no more than they belong to me — or you.
To add insult to injury, Getty Images listed itself/Carol Highsmith as these works’ creator, which suggests that she was in cahoots with them, notwithstanding that Highsmith first learned of this scam when she received a threatening letter for not paying licensing fees for the privilege of using her own pictures on her own website.
Yes, the mind boggles.
Then I wondered: if Getty Images is pretending that they have the right to demand payment for the use of Highsmith’s photos, could they be pulling the same scam with other images in the public domain?
It took less than an hour to establish that Gettying extends beyond the Highsmith experience. Consider these 2 pictures of ships. What’s the difference? Unless you want to place it in an advertisement, using the first image is free — no licensing, no permissions.

 In contrast, this photo, the one with “gettyimages/ US Navy” will cost you $575 to use.
In contrast, this photo, the one with “gettyimages/ US Navy” will cost you $575 to use.
Even the caption at Getty is plagiarized — stolen — from the US Navy.
Compare http://www.gettyimages.com/license/612905348 to the screenshot above from the Navy:
“Ships Huddle At Key West To Offer Aid As Hurricane Matthew Approaches
Credit: U.S. Navy / HandoutEditorial #: 612905348Collection: Getty Images NewsKEY WEST, FL – OCTOBER 5: Nine ships from the Royal Bahamas Defence Force, research vessel Walton Smith and a contract vessel take shelter at Naval Air Station Mole Pier as Hurricane Matthew approaches October 5, 2016 in Key West, Florida. NAS Key West is not currently projected to be in Matthew’s path and as such, stands by to support other services and relief efforts. NAS Key West is a state-of-the-art facility for air-to-air combat fighter aircraft of all military services and provides pierside support to U.S. and foreign naval vessels. (Photo by Cody R. Babin/U.S. Navy via Getty Images)”.
The US Navy website makes it clear that you need not pay licensing fees:
Notice: U.S. Navy photographs and digital images on this site are fully released by the U.S. Navy. If used for news and information purposes please credit as “U.S. Navy photo by [photographer’s name].” The use of Navy images for advertisements must be specifically approved by the Navy Office of Information (OI-2) prior to the use. Write to navymedia@navy.mil and include details on your intended usage.
In other words, unless you want to use the picture of the ship at Key West in an advertisement, you are free to do so for free. The idea is that since the military is supported by tax dollars, you have already paid for this picture.
And let’s be clear about this: Mass Communication Specialist 3rd Class Cody R. Babin is not working for Getty Images. He is not paid by them. He works for us. Really, he ought to protest the use of his name by Getty because were he on both their payroll and the Navy’s, he would be double-dipping. Yes, I suppose it is nice of Getty to acknowledge him as the creator of the work — but do you think he will see one thin dime of the $575 licensing fee Getty is charging for — well, for what?
Next up: Gettying NASA photos and historical images from the Library of Congress.
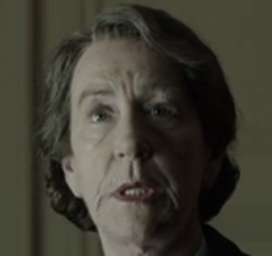
Foyle’s War’s Teeth
Perhaps it was by design, or perhaps not, but the attention to period detail in the crime series Foyle’s War is remarkable and rare in a seemingly simple way: it gets teeth right.
Foyle’s War is a police drama featuring Detective Superintendent Christopher Foyle (Michael Kitchens). Many of the crimes he investigates in Hastings, Sussex during WWII are related to the conditions on the homefront including profiteering and sabotage, but jealousy and madness also provoke ordinary people to behave wickedly. The show premiered in 2002 and ended in 2015 after 28 90-minute episodes. The last episodes following the war find Foyle in London, working for MI5.
Foyle is a quiet, highly principled man. He is compassionate, but he does not suffer fools. He’s a widower with one son, Andrew, serving in the RAF. From the first episode onwards he is accompanied by Samantha Stewart (Sam) as his driver, and in the first five seasons he works with Sgt. Milner, a policeman who lost part of a leg in the war.
There are perhaps a half dozen other characters who appear in more than one episode, but for the most part, the cast is fluid.
Its creator, Anthony Horowitz, has attributed Foyle’s War appeal to the tone of the show. It defies the sentimental nostalgia for the war years, and Horowitz based many of the situations Foyle investigates on historical events. The New York Times acknowledges that Foyle’s War is typically “celebrated for the ‘historical accuracy’ (those are the words always used) achieved by its creator and writer, Anthony Horowitz. . . . The better word is probably scrupulousness — the special texture of the show owes to the faith we feel in Mr. Horowitz’s depiction of the clamped-down, suspicious yet doughty atmosphere of 1940s Britain, and to the trouble and expense to which the production has gone to recreate those times.”
In contrast, consider the criticism of Downton Abbey, which historian A. N. Wilson called a “sanitized fantasy.” Downton may get the place settings right, but “the servants in the program are far too clean,” according to historian Jennifer Newby: “The reality would have been a lot more grubby, I don’t think people realize that the servants stank.”
All I think you need to do to understand why Downton is fantastical and Foyle’s War is not, is to look at the teeth.

Christopher Foyle (Michael Kitchen) has acceptable, ordinary teeth. There are no obvious flaws, other than a little yellowing. Foyle smiles easily – he has a very expressive face – but his smiles are usually closed.
Samantha (Sam) Stewart (Honeysuckle Weeks). Sam’s mouth seems to change from the start of the series to its final episodes. In the opening episodes, Sam’s teeth seem to be a bit small for her mouth and there appear to be spaces between her teeth.
In the last series, her teeth seem capped and bonded.

Sgt. Milner has good teeth, as does Foyle’s son, Andrew. The actors who portray them, Anthony Howell and Julian Mark Ovenden, were stage actors. I expect it would have been hard to find experienced actors to play young men in their twenties who have not had good dentistry.
What’s interesting is that the characters who have obvious problems with their teeth represent all social classes. A fisherman, a police commissioner, doctors, army brass, industrialists – all are at risk. Not everyone has bad teeth: a daughter of a wealthy family in Series 1, episode 1, has perfect teeth, as does a burn victim.
Let’s see some examples:









Some do have good teeth:
I don’t know if in the between-the-wars period imperfect teeth could be fixed to look like what is considered normal today, but the family of Downton Abbey would have had the resources for cosmetic dentistry if needed and available. So it isn’t too surprising that Lady Mary, Mrs. Crawley, and the rest of the Granthams have 21st century American teeth.
But it would be very surprising if the servants of the house also have perfect smiles. And they do. This is a huge oversight for a series that claims to be true to its historical period.




Let’s face it: imperfect teeth are taboo. There can be no glamour when there’s a crooked tooth.
But there can be no pretense of historical accuracy when the scullery maid has a smile that rivals an aristocrat’s.
The Audacity of Getty Images Exploiting Carol Highsmith, America’s Photographer
I first wrote about Carol Highsmith eight years ago, asking “Is Carol M. Highsmith the Most Generous Artist of Our Time?” The answer was yes then and remains so today. Others agree with this valuation, including C. Ford Peatross, director of Architecture, Design and Engineering, Prints and Photographs, Library of Congress, who in 2007 remarked: “The donation of her photographs [The Highsmith (Carol M.) Archive] is one of the greatest acts of generosity in the history of the Library.”
Highsmith has provided the Library of Congress with 31,828 images (as of today, 8/18/16)– and has stipulated that they be placed in the public domain. The Library expects that number will likely approach 100,000.
I was astounded to find an outstanding contemporary photographer’s work could be freely used. No licensing fees are required to use her images, but there should be a credit line, at the least identifying her as the Creator of the work, and preferably using this Credit Line: Library of Congress, Prints & Photographs Division, photograph by Carol M. Highsmith [reproduction number, e.g., LC-USZ62-123456].
After I posted the first time about Highsmith, I learned she was seeking sponsors for an ambitious project, photographing every state so that a record may be had of what America looked like in the first decades of the 21st century. I’ve been following her progress since she started with Alabama, with sponsorship from philanthropist George F. Landegger.
You can imagine how appalled I was to read about the gross exploitation of Highsmith’s generosity by Getty Images.
In December 2015 Highsmith received notification from Alamay Ltd.’s License Compliance Services (LCS), (on behalf of Getty Images) demanding $120 because she was in breach of Getty’s licensing terms for the content of an image she had used on her website and accusing her of copyright infringement.
The image in question: one of Highsmith’s own and one she placed in the Library of Congress with the stipulation that it be placed in the public domain.
Apparently, Getty Images had been downloading her thousands of images, placing them on its site, and demanding licensing fees, as if Getty owned the images. In other words, they were doing exactly the opposite of Highsmith’s intention, which is to allow free use of her images. Using her images is not the same as owning her images.
Getty had 18,755 of Highsmith’s photos on its site.
The way this all came to light was because Getty “scrapes” the net, looking for uses of its images and checking license fees have been paid.
Eventually the scraper hit Highsmith’s website, and the scheme was exposed. Perhaps if Getty had been careful to credit Highsmith as the photographer, they would have realized sending Highsmith a threatening letter wasn’t a good idea.
Highsmith has filed a $1 billion dollar suit.
Writing for Forbes.com, IP specialist Attorney Bryan Sullivan summarizes the suit:
“against Getty Images targeting the ‘gross misuse’ of 18,755 of Highsmith’s photographs. According to the suit, ‘The defendants [Getty Images] have apparently misappropriated Ms. Highsmith’s generous gift to the American people…. [They] are not only unlawfully charging licensing fees but are falsely and fraudulently holding themselves out as the exclusive copyright owner.’ Highsmith claims that Getty was unlawfully telling users that they would have to buy a copyright license from Getty to use the images. ‘Likewise, nowhere on its website does Getty identify Ms. Highsmith as the copyright owner of the work.’”
Sullivan expects Getty will settle out of court.
A prediction: when she wins, Highsmith’s life will change in one way. She won’t have to seek sponsorships to make it possible for her to work night and day, and this means she’ll have more time to document America.
You can follow Highsmith’s travels on Facebook (Carol M. Highsmith’s America).
Here are four of Highsmith’s photos: “Porter Sculpture Park, Montrose, South Dakota,” “Alpine lakes and forest, Denali National Park, Alaska,” “Monument Valley View, Arizona,” and “July 4th fireworks, Washington, D.C.”



Credits: Library of Congress, Prints & Photographs Division, photographs by Carol M. Highsmith [ LC-DIG-highsm-04547, LC-DIG-highsm-04272, LC-DIG-highsm-04002, LC-DIG-highsm-04460]






